In North Carolina, as in much of America, coronavirus cases are on the rise again. Nash County, a largely rural area in the north of the state, hasn’t yet been overwhelmed by the pandemic. But people there are anxious about the persistence of the virus and uncertain about the road […]
BALTIMORE — In the raging national debate over whether to reopen schools, advocates on both sides are basing their arguments on a range of factors: political, economic and emotional. But there is a growing consensus in the public health and scientific community that schools should resume in-person classes this fall […]
President Donald Trump’s newfound disdain for online education is a sharp departure from what his administration and Education Secretary Betsy DeVos have long championed in terms of policy on virtual learning. As he presses schools and colleges to physically reopen their doors this fall, Trump has dismissed online learning as […]
It was another troubling week in California, as growing infections and hospitalizations prompted state and local officials to announce new widespread closures of businesses and schools across the state to slow the coronavirus pandemic. The pandemic, which is disproportionately ravaging communities of color, has killed at least 7,475 Californians. This […]
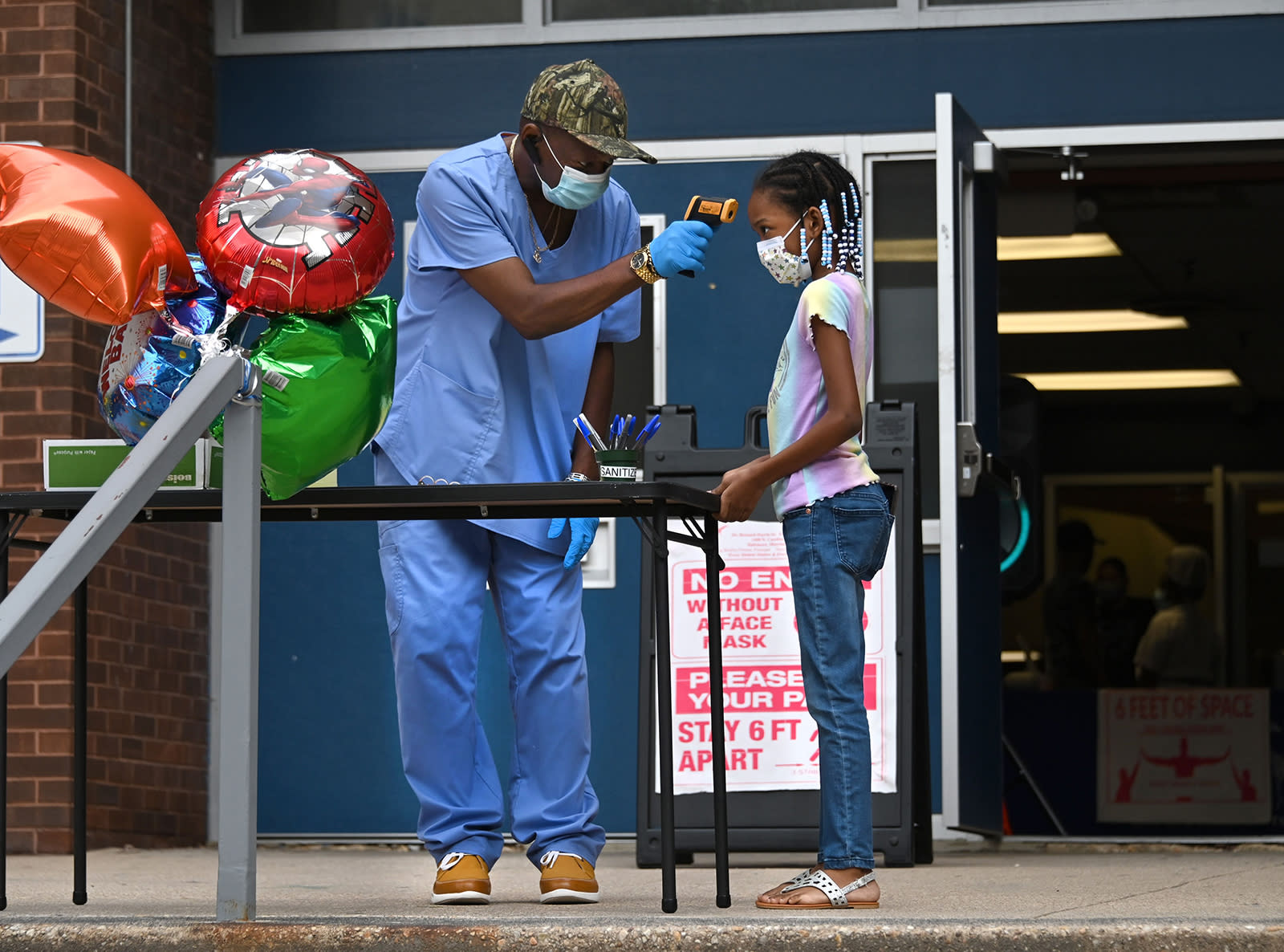
EAST COBB, GA — Cobb County’s schools joined other area districts Thursday in announcing that fall classes would be online only. Speaking to the Cobb County Board of Education in an online meeting, Superintendent Chris Ragsdale said he made the decision because “we didn’t have any more information than the […]
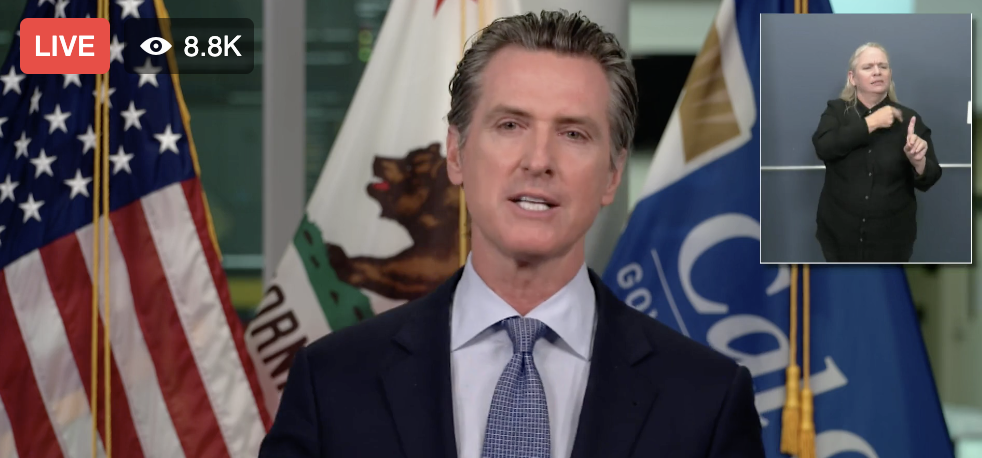
NAPA COUNTY, CA — If Napa County is still on the state of California’s COVID-19 coronavirus watchlist when the fall semester begins, Napa Valley Unified School District and other districts within the county will have to start the school year with online classes, Gov. Gavin Newsom announced Friday. Counties where […]
Click here to read the full article. At his Friday news conference, California Governor Gavin Newsom ordered counties on the state’s coronavirus watch list to shut down school campuses this fall, at least to begin the school year. The 32 counties on the list — which include Los Angeles and […]
HILLSBOROUGH COUNTY, FL — She’s the mom of a 13-year-old son with pre-existing medical conditions and an elementary school teacher. That makes Ariane Hargrave of Apollo Beach doubly skeptical about plans to reopen Hillsborough County public schools next month. Hargrave said any viral illness exacerbates her son’s severe asthma “to […]